
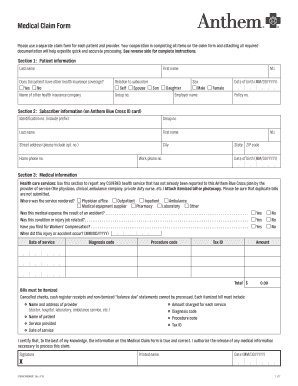
If the member’s eligibility cannot be identified, the provider will receive notification via voucher designated “PAUNK.” The member’s name will be included on this voucher so that the provider can research and resubmit if necessary. Providers will receive notification of claims payment or denial via check and remittance advice. You can recreate a claim and submit it as a replacement or cancellation (void) of the original claim, if Anthem Blue Cross and Blue Shield (Anthem) has already accepted the original claim for processing. Availity Portal corrected claim submission.

A clean claim is a claim received by Carelon with all required data present and valid that was adjudicated without having to obtain information from an external source. As a reminder, t he corrected claim must be received within the timely filing.
Carelon’s standards for claim turnaround time are to pay “clean claims” within 30 days of initial receipt.

You must resubmit a corrected claim for any claims. Claims that are not submitted within the 90-day timeframe will not be considered for reimbursement. Please also refer to diagnosis-specific processing information later in this handbook. What is Anthem timely filing for corrected claims The corrected claim must be received within the timely filing limit due to the initial claim not being. Title: TXAGP-MMP-RP-017193-22-CPN16502 Claims Timely Filing BRFINAL.docx Author: Robyn M. Corrected Claims Eligible Billed Charges. Anthem Blue Cross Blue Shield Timely filing limit - BCBS TFL List Ambetter Timely Filing Limit Workers Compensation. However, we encourage providers to submit claims on a monthly basis. standard timely filing limits will be denied as outside the timely filing limit. Cigna has sought to abandon the merger and force Anthem to pay a $1.85 billion breakup fee while Anthem filed a lawsuit to force its smaller rival to go through with the combination.Īnthem and the Justice Department did not immediately respond to a request for comment on the appeals court decision.All claims must be submitted within ninety (90) days of the discharge date or date of service. Availity Portal corrected claim submission You can recreate a claim and submit it as a replacement or cancellation (void) of the original claim, if Anthem Blue Cross and Blue Shield (Anthem) has already accepted the original claim for processing. In another obstacle to the deal, Anthem and Cigna are suing each other. The following are corrected claim filing limits provided as days and begin on the date services are rendered, unless otherwise noted. As a reminder, t he corrected claim must be received within the timely filing. The notice also hints at the possibility of negotiating the time frame but makes it clear they are prepared to lose some contracted providers over the amendment.
“This is a red letter day for consumers,” said David Balto, who organized opposition to the deal. This means all claims submitted on or after Octowill be subject to a ninety (90) day timely filing requirement, states the announcement. Kavanaugh argued that a combined Anthem/Cigna would require higher payments to manage the accounts but that would be offset by better negotiated rates paid to providers.Īnthem, a member of the Blue Cross Blue Shield Association, is the second biggest seller of medical insurance to big U.S. In a dissent, Judge Brett Kavanaugh argued that the merger would benefit the biggest customers, mainly large companies with employees in many states.


 0 kommentar(er)
0 kommentar(er)
